Alcohol After Gastric Bypass: Liver Damage Risks
We delve into the intricate relationship between gastric bypass surgery, alcohol consumption, and liver damage. By understanding the risks involved and implementing preventive measures, patients can navigate their post-surgery journey with greater awareness and ensure the long-term health of their liver and overall well-being.
Understanding Gastric Bypass and Alcohol
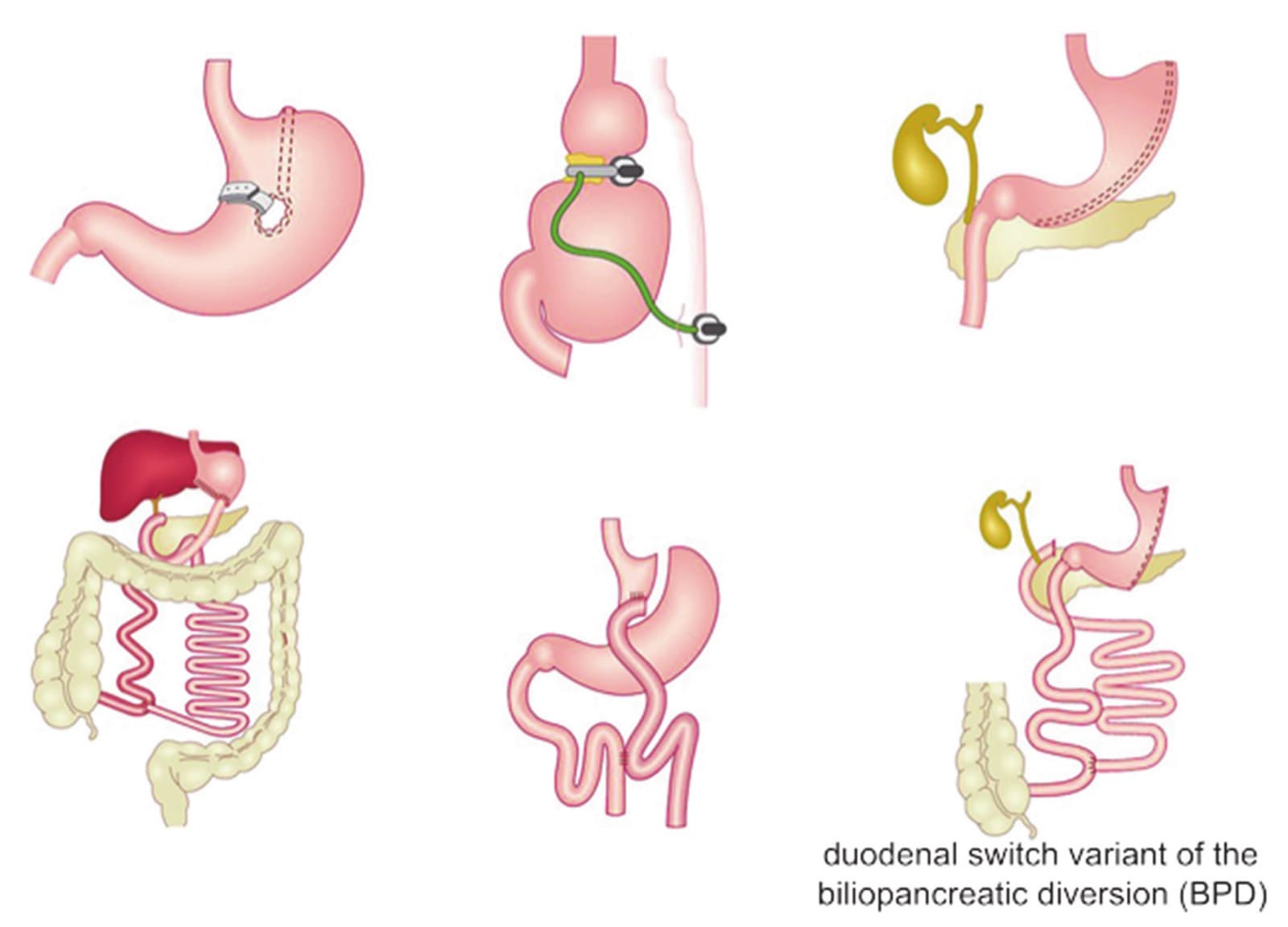
Gastric bypass surgery is a weight loss procedure that involves reducing the size of the stomach and rerouting the digestive system. This surgery is often performed on individuals who are severely obese and have been unable to lose weight through other methods such as diet and exercise.
When it comes to alcohol consumption after gastric bypass surgery, there are a few important considerations:
- Alcohol Absorption: After gastric bypass surgery, the stomach is smaller and the small intestine is rerouted. This can lead to changes in how alcohol is absorbed and metabolized in the body. The smaller stomach means that alcohol may be absorbed more quickly into the bloodstream, leading to a higher blood alcohol concentration;
- Increased Sensitivity: Due to changes in alcohol absorption and metabolism, individuals who have undergone gastric bypass surgery may become more sensitive to the effects of alcohol. This means that they may feel the effects of alcohol more quickly and intensely than they did before surgery;
- Nutritional Concerns: Alcohol provides empty calories and lacks essential nutrients. After gastric bypass surgery, individuals are often advised to focus on nutrient-dense foods to prevent deficiencies. Consuming alcohol may displace these nutrient-dense foods and contribute to nutritional deficiencies if not consumed in moderation;
- Potential for Addiction: Some studies suggest that individuals who have undergone gastric bypass surgery may be at a higher risk for developing alcohol use disorder or experiencing alcohol-related problems. This could be due to changes in alcohol metabolism or psychological factors related to the surgery and weight loss;
- Consultation with Healthcare Provider: It’s essential for individuals who have undergone gastric bypass surgery to discuss alcohol consumption with their healthcare provider. They can provide personalized advice based on the individual’s health status, weight loss goals, and any potential risks associated with alcohol consumption.
In summary, while moderate alcohol consumption may be acceptable for some individuals after gastric bypass surgery, it’s important to be mindful of changes in alcohol absorption and metabolism, as well as potential nutritional concerns and risks for alcohol-related problems. Consulting with a healthcare provider is crucial for personalized guidance and recommendations.
The Risks of Alcohol Consumption After Gastric Bypass
Alcohol consumption after gastric bypass surgery carries several potential risks due to changes in the digestive system and metabolism. Here are some of the risks associated with alcohol consumption after gastric bypass:
- Increased Intoxication: With a smaller stomach pouch and altered gastrointestinal anatomy, alcohol is absorbed more rapidly into the bloodstream. This can lead to quicker intoxication and higher blood alcohol levels compared to before the surgery. Individuals may feel the effects of alcohol more quickly and intensely, increasing the risk of accidents or alcohol poisoning;
- Nutritional Deficiencies: Alcohol provides empty calories and lacks essential nutrients. After gastric bypass surgery, individuals need to prioritize nutrient-dense foods to prevent deficiencies. Drinking alcohol can displace these important nutrients and contribute to malnutrition if consumed regularly or in large amounts;
- Dumping Syndrome: Gastric bypass surgery can lead to dumping syndrome, a condition characterized by rapid emptying of the stomach contents into the small intestine. Consuming alcohol can trigger dumping syndrome symptoms such as nausea, vomiting, diarrhea, abdominal cramps, sweating, and dizziness. These symptoms can be uncomfortable and may discourage further alcohol consumption;
- Risk of Addiction: Some studies suggest that individuals who have undergone gastric bypass surgery may be at an increased risk of developing alcohol use disorder or experiencing alcohol-related problems. Changes in alcohol metabolism and the psychological impact of rapid weight loss may contribute to an increased vulnerability to alcohol addiction;
- Interaction with Medications: After gastric bypass surgery, individuals may be prescribed medications for various reasons. Alcohol can interact with these medications, leading to adverse effects or reducing the effectiveness of the medications. It’s crucial for individuals to consult with their healthcare provider regarding potential interactions between alcohol and any prescribed medications;
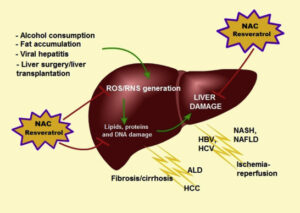
- Worsening of Health Conditions: Alcohol consumption can exacerbate certain health conditions, such as liver disease, diabetes, and hypertension, which may already be present in individuals who have undergone gastric bypass surgery. Excessive alcohol intake can further strain the liver and worsen metabolic control, leading to complications;
- Psychological Impact: Alcohol consumption can affect mood and cognition. Individuals who have undergone gastric bypass surgery may be more susceptible to the psychological effects of alcohol due to changes in brain chemistry and sensitivity to alcohol. This can potentially increase the risk of depression, anxiety, or other mental health issues.
Overall, while moderate alcohol consumption may be tolerated by some individuals after gastric bypass surgery, it’s essential to be aware of the potential risks and to exercise caution. Consulting with a healthcare provider before consuming alcohol is advisable, and individuals should be mindful of their alcohol intake and its effects on their health and well-being.
Preventing Alcohol-Related Liver Damage After Gastric Bypass
Preventing alcohol-related liver damage after gastric bypass surgery is crucial for the long-term health and well-being of individuals who have undergone this procedure. Here are some steps that can help mitigate the risk of liver damage associated with alcohol consumption after gastric bypass:
- Limit Alcohol Consumption: The most effective way to prevent alcohol-related liver damage is to limit or avoid alcohol consumption altogether. Following gastric bypass surgery, individuals should adhere to the recommended guidelines for alcohol intake provided by their healthcare provider. This typically means consuming alcohol in moderation or abstaining from it entirely;
- Understand Alcohol Guidelines: Healthcare providers may provide specific recommendations regarding alcohol consumption after gastric bypass surgery. These guidelines may include limits on the amount of alcohol that can be safely consumed, advice on spacing out drinks, and suggestions for avoiding high-alcohol-content beverages;
- Monitor Liver Health: Regular monitoring of liver function through blood tests can help detect early signs of liver damage or dysfunction. Individuals who have undergone gastric bypass surgery should follow up with their healthcare provider as recommended to assess liver health and address any concerns promptly;
- Maintain a Healthy Lifestyle: Adopting and maintaining a healthy lifestyle can support liver health and reduce the risk of alcohol-related liver damage. This includes maintaining a balanced diet, engaging in regular physical activity, staying hydrated, and avoiding other risk factors for liver disease such as smoking and excessive consumption of processed foods or sugary beverages;
- Avoid Binge Drinking: Binge drinking, defined as consuming a large amount of alcohol in a short period, can significantly increase the risk of liver damage and other health problems. Individuals who have undergone gastric bypass surgery should be particularly cautious to avoid binge drinking and pace their alcohol consumption to minimize the impact on the liver and overall health;
- Be Aware of Symptoms: It’s essential to be aware of the signs and symptoms of liver damage, which may include fatigue, abdominal pain or swelling, jaundice (yellowing of the skin or eyes), dark urine, and unexplained weight loss. If any concerning symptoms arise, individuals should seek medical attention promptly;
- Seek Support and Counseling: Individuals who struggle with alcohol consumption after gastric bypass surgery may benefit from seeking support and counseling. This could include participation in support groups, therapy, or counseling sessions focused on addressing alcohol use and developing healthy coping strategies.
Overall, preventing alcohol-related liver damage after gastric bypass surgery requires a combination of education, lifestyle modifications, monitoring, and support. By being mindful of alcohol intake and taking proactive steps to support liver health, individuals can reduce the risk of liver damage and maintain overall well-being following surgery.
Conclusion
Navigating the intersection of gastric bypass surgery and alcohol consumption requires vigilance, understanding, and proactive measures. As patients embark on their weight loss journey post-surgery, it’s paramount to prioritize liver health and acknowledge the potential hazards associated with alcohol intake.
By embracing informed decision-making, adopting healthy lifestyle practices, and seeking support from healthcare professionals and support networks, individuals can mitigate the risks of alcohol-related liver damage and pave the way for sustained well-being. Remember, the journey to optimal health post-gastric bypass is multifaceted, and safeguarding liver health serves as a cornerstone for long-term success and vitality. Let knowledge guide your choices, and may your path be illuminated with wellness and resilience.