LDLT Medical Abbreviation: A Detailed Review
Unveiling the LDLT Medical Abbreviation
Are you acquainted with the transformative medical intervention termed living donor liver transplantation (LDLT)? This innovative approach has revolutionized the field of organ transplants, bringing renewed hope and vitality to individuals in dire need of a healthy liver.
In this comprehensive exploration, we delve into the specifics of living donor liver transplantation, highlighting the process, benefits, and profound effect on both donors and recipients. This narrative offers an all-encompassing look at the procedure, from the selection of donors to the surgical details and recovery journey. It’s a guide for those considering donation options or curious about the surgery’s nuances, providing a clear understanding of this life-saving medical intervention. Join us as we uncover the complexities of these transplants, shedding light on a topic of critical importance to many.
Demystifying Living Donor Liver Transplant (LDLT)
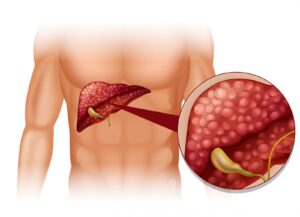
LDLT, an acronym for Living Donor Liver Transplant, emerges as a beacon of hope amidst the scarcity of available organs from deceased donors. The practice involves the donation of a segment of a healthy liver by a living donor, a process that significantly accelerates the recovery phase post-transplant and subsequently increases the survival rate of the recipient.
The procedure entails the surgical removal of part of the donor’s liver and its transplantation into a recipient suffering from liver failure. Remarkably, the liver tissue of both the donor and recipient regenerates, eventually reaching its full size again.
Potential living liver donors undergo a rigorous screening process to confirm their eligibility. This process includes assessments of physical health and compatibility of blood type with the recipient. The willingness to donate a portion of one’s liver embodies a profound act of generosity and empathy, as it involves personal health risks to aid another person’s survival.
Delving Into the Living Donor Liver Transplant Surgery

The operation of LDLT unfolds through several intricate phases, which we will elucidate sequentially:
- Initial Assessment: Candidates for living donation are thoroughly screened, encompassing a review of their health history, a physical examination, and evaluations of liver functionality before the operation;
- Operative Steps: In this delicate process, the donor’s liver is divided into two parts: the right and left lobes. The recipient typically receives the larger right lobe, while the donor retains the smaller left lobe;
- Vascular and Biliary Reconnection: The transplant team carefully joins the blood vessels and bile ducts of the donor liver portion to those of the recipient, ensuring the transplanted liver has adequate blood flow and bile drainage;
- Post-Surgical Care and Observation: Following the surgery, both the donor and recipient are closely observed and allowed time to recover to confirm the transplant’s effectiveness;
- Liver Regrowth: The liver sections in both the donor and recipient gradually grow back, reaching their original volume, which helps in regaining liver function and improving overall health.
Understanding a Partial Liver Transplant
- Procedure Description: In a split liver transplant, a segment of the donor’s liver is surgically removed and transplanted into another individual;
- Segmentation for Transplant: The donor’s liver is split into two lobes, left and right. Generally, the left lobe is allocated to a pediatric recipient, whereas the right lobe is reserved for an adult;
- Ensuring Functional Integration: The operation includes precise linkage of the donor liver’s blood vessels and bile ducts with the recipient’s, critical for maintaining liver function post-transplant;
- Regenerative Ability: The donor’s remaining liver tissue undergoes regeneration, reestablishing full liver functions for both the donor and recipient over time;
- Post-Transplant Recovery: The remarkable regenerative capacity of the liver makes transplantation a viable last-resort treatment for end-stage liver disease, allowing both parties to regain health and lead productive lives after the procedure.
Blood Type Compatibility in Liver Transplant

There are four main blood types – A, B, AB, and O, each of which can be positive or negative. The transplantation compatibility between blood types follows a specific pattern:
| Donor / Recipient | A | B | AB | O |
|---|---|---|---|---|
| A | Yes | No | Yes | No |
| B | No | Yes | Yes | No |
| AB | No | No | Yes | No |
| O | Yes | Yes | Yes | Yes |
It’s critical to note that compatibility is influenced by the Rh factor, which determines whether a person’s blood type is positive or negative. Blood type compatibility is meticulously analyzed during the evaluation phase to ensure a successful transplantation with reduced risk of organ rejection.
LDLT Statistics
There are several prerequisites for individuals to be considered as potential donors:
- Good physical and mental health: Donors need to be in good overall health and devoid of major medical conditions that could impact their ability to undergo surgery;
- Compatible blood type: Donors should show blood type compatibility with the recipient to minimize organ rejection risks;
- Liver compatibility: The anatomy and size of the donor’s liver must be suitable for transplantation and capable of adequately supporting the recipient’s liver function;
- Voluntary and informed consent: Donors should willingly opt to donate and understand the potential risks and complications associated with the surgery.
It’s important to remember that the decision to donate should be a personal one, made after thoughtful deliberation and consultation with healthcare professionals and family.
Preconditions to Consider Before Donating
Before becoming a living liver donor, it’s crucial to consider a few prerequisites:
- Age restrictions: Generally, donors must be between 18 and 60 years old;
- Body Mass Index (BMI): Donors should have a BMI within a healthy range, generally less than 30;
- Economic considerations: The process involves time off work for recovery. Therefore, prospective donors should have a plan for dealing with potential lost wages;
- Understanding the risk: Every surgery involves risk, and a living donor liver transplant is no exception. Potential donors must understand these risks before making a decision.
The Impact of LDLT on the Donor and Recipient
Living donor liver transplant has significant consequences, both physical and emotional, for the donor and the recipient. Here are a few impacts worth discussing:
- For the donor: Potential risks and drawbacks include surgical complications, discomfort during recovery, and a small chance of longer-lasting complications. On the other side, donors often express a sense of fulfillment and purpose, knowing they played a part in saving a life;
- For the recipient: The waiting time for a transplant is substantially reduced, as is the deterioration of the health often experienced while waiting for a deceased donor organ. The quality of the organ is usually better, as the healthy liver segment comes from a living, healthy individual.
As the demand for liver transplants escalates, raising awareness about LDLT and promoting organ donation is paramount. If you or a loved one requires a liver transplant, consider reaching out to professional entities or healthcare providers.
Frequently Asked Questions
A living donor liver transplant employs a segment from a healthy donor, contrasting with transplants that use organs from deceased donors. This approach significantly reduces wait times and improves results, thanks to the quick availability of a compatible organ.
Typically, living donors for liver transplants are either close relatives or emotionally linked individuals who wholeheartedly choose to donate a share of their liver. They need to undergo a thorough evaluation to ensure compatible blood type and confirm their good health prior to surgery.
The liver exhibits an exceptional regenerative capacity. Upon a living donor liver transplant, both the donor’s residual liver and the recipient’s transplanted liver portion regenerate and grow. This regrowth leads to the restoration of normal liver functions in both individuals.
LDLTs offer multiple benefits such as reduced waiting times for transplantation, better outcomes due to the use of a healthy liver, convenience of planning the surgery, and potentially faster recovery compared to deceased donor transplants. Moreover, the altruistic act of a living donor can save a life, further bolstering the emotional connection between the donor and the recipient.
Conclusion
LDLT stands as a pivotal solution for those grappling with critical liver ailments, granting a renewed opportunity for health. This sophisticated method utilizes a segment from a willing, healthy donor, addressing the dire shortage of organs available from deceased donors. With the benefits of shorter waiting periods and improved success rates due to the prompt availability of compatible organs, LDLT represents a significant advancement in transplantation. Rigorous screening processes are in place to ascertain the suitability of candidates, focusing on both the donor’s and recipient’s well-being. As knowledge and understanding of this option expand, its capacity to save lives becomes increasingly evident. Thus, for individuals contemplating a transplant, exploring LDLT could be a transformative decision.