Metformin’s Liver Enzyme Interaction
Metformin stands as a cornerstone in the treatment of type 2 diabetes, hailed for its efficacy in controlling blood sugar levels and improving insulin sensitivity. Amid its widespread use, questions arise regarding its impact on liver function, a vital concern given the organ’s central role in metabolism and drug processing.
Understanding the interplay between metformin and liver function is crucial for optimizing patient care and ensuring the medication’s safe and effective use. In this comprehensive guide, we delve into the mechanisms of metformin’s action, explore its effects on liver enzymes, and address key safety considerations to empower individuals and healthcare providers with valuable insights into metformin therapy.
What are Liver Enzymes?
Liver enzymes are proteins produced by the liver cells, known as hepatocytes, that play a crucial role in various metabolic processes within the body. These enzymes are involved in facilitating chemical reactions necessary for breaking down substances like drugs, toxins, and nutrients. They also aid in the synthesis and metabolism of proteins, carbohydrates, and fats.
Liver enzymes are typically measured through blood tests, and the levels of specific enzymes can provide valuable insights into liver health. The main liver enzymes commonly measured in blood tests include:
- Alanine aminotransferase (ALT): ALT is primarily found in the liver and is released into the bloodstream when liver cells are damaged. Elevated ALT levels are often indicative of liver injury or disease, such as hepatitis or fatty liver disease;
- Aspartate aminotransferase (AST): Like ALT, AST is an enzyme found predominantly in the liver and is released into the bloodstream when liver cells are damaged. Elevated AST levels can signal liver damage, although AST levels can also rise due to heart or muscle damage;
- Alkaline phosphatase (ALP): ALP is an enzyme found in various tissues throughout the body, including the liver, bones, and bile ducts. Elevated ALP levels may indicate liver or bone disorders, such as liver obstruction or bone disease;
- Gamma-glutamyl transferase (GGT): GGT is found in the liver and other tissues, including the kidneys and pancreas. Elevated GGT levels can be a marker of liver or bile duct injury, as well as alcohol consumption or certain medications.
Monitoring liver enzyme levels through blood tests can help healthcare providers assess liver function, diagnose liver diseases, and monitor the effects of medications or treatments on the liver. However, it’s essential to interpret liver enzyme results in the context of the individual’s overall health and medical history, as elevated levels can be caused by various factors other than liver disease.
How Metformin Works

Metformin is a medication commonly prescribed to manage type 2 diabetes, a condition characterized by high blood sugar levels due to insulin resistance or inadequate insulin production. Understanding how metformin works is essential for comprehending its therapeutic effects.
- Reducing Glucose Production: One of the primary mechanisms of metformin involves inhibiting glucose production in the liver. The liver normally produces glucose through a process called gluconeogenesis, where it converts stored forms of energy (glycogen and fats) into glucose. Metformin suppresses this process, thereby decreasing the amount of glucose released into the bloodstream;
- Improving Insulin Sensitivity: Metformin also enhances the sensitivity of peripheral tissues, such as muscle and fat cells, to insulin. Insulin is a hormone that helps cells absorb glucose from the bloodstream for energy. In individuals with insulin resistance, cells do not respond effectively to insulin, leading to elevated blood sugar levels. By improving insulin sensitivity, metformin enables cells to take up glucose more efficiently, thereby reducing blood sugar levels;
- Decreasing Intestinal Glucose Absorption: Additionally, metformin may decrease the absorption of glucose from the intestines after meals. By limiting the amount of glucose entering the bloodstream from the digestive system, metformin contributes to overall blood sugar control;
- Modulating Gut Microbiota: Emerging research suggests that metformin may exert some of its effects through interactions with the gut microbiota—the diverse community of microorganisms residing in the gastrointestinal tract. Metformin may alter the composition and function of gut bacteria, which can influence metabolic processes and inflammation, contributing to its therapeutic effects;
- Potential Effects on AMPK: Metformin’s primary molecular target within cells is believed to be an enzyme called AMP-activated protein kinase (AMPK). Activation of AMPK plays a crucial role in regulating cellular energy metabolism, including glucose uptake, fatty acid oxidation, and mitochondrial biogenesis. By activating AMPK, metformin promotes cellular energy balance and insulin sensitivity.
Overall, metformin’s multifaceted mechanisms of action make it a cornerstone therapy for managing type 2 diabetes. By targeting various pathways involved in glucose metabolism and insulin sensitivity, metformin helps to lower blood sugar levels and improve metabolic health in individuals with diabetes. However, it’s important to note that metformin is typically used as part of a comprehensive treatment plan that may include lifestyle modifications, such as diet and exercise, as well as other medications as needed.
Metformin and Liver Function
Metformin, a widely prescribed medication for managing type 2 diabetes, has garnered attention for its potential impact on liver function. Understanding the relationship between metformin and liver function is crucial for individuals using this medication and their healthcare providers.
Metformin and Liver Enzymes
One area of interest regarding metformin’s effects is its potential impact on liver enzymes. Liver enzymes, such as alanine aminotransferase (ALT) and aspartate aminotransferase (AST), are markers of liver health. Elevated levels of these enzymes can indicate liver damage or disease.
Studies have shown that metformin use may lead to changes in liver enzyme levels, although the findings are mixed. Some research suggests that metformin use may cause a slight increase in liver enzyme levels, particularly in the initial stages of treatment. However, these elevations are often mild and transient, and they typically do not indicate significant liver damage.
On the contrary, other studies have found that metformin use is associated with lower liver enzyme levels, suggesting potential beneficial effects on liver function. These findings highlight the complex relationship between metformin and liver enzymes, and more research is needed to fully understand the mechanisms involved.
Safety Considerations
Overall, metformin is considered safe and well-tolerated for most people with type 2 diabetes. However, certain individuals may be at higher risk of adverse effects, particularly those with pre-existing liver disease or impaired liver function.
Before starting metformin therapy, healthcare providers typically assess liver function through blood tests to ensure that the medication can be safely prescribed. Additionally, regular monitoring of liver enzyme levels may be recommended during metformin treatment to detect any changes and address them promptly.
It’s essential for individuals taking metformin to communicate openly with their healthcare providers about any concerns or symptoms they experience, especially those related to liver health. By working together, healthcare providers and patients can ensure the safe and effective use of metformin while monitoring its effects on liver function.
Research Findings
Studies investigating the effects of metformin on liver enzymes have yielded mixed results. Some research suggests that metformin may lead to a slight increase in liver enzyme levels, particularly alanine aminotransferase (ALT) and aspartate aminotransferase (AST), which are markers of liver damage when elevated. However, these elevations are often mild and transient.
On the contrary, other studies have found that metformin use is associated with lower liver enzyme levels, indicating potential beneficial effects on liver function. These conflicting findings highlight the complexity of the relationship between metformin and liver enzymes.
Clinical Implications
For individuals with diabetes or other metabolic conditions, monitoring liver enzyme levels is essential, especially when initiating or adjusting metformin therapy. Healthcare providers may recommend periodic liver function tests to assess liver health and ensure the safe use of metformin.
Safety Considerations
Safety considerations are paramount when prescribing and using metformin, especially considering its widespread use in managing type 2 diabetes. While metformin is generally considered safe and well-tolerated, certain precautions and considerations should be kept in mind:
- Kidney Function: Metformin is primarily excreted through the kidneys. Therefore, individuals with impaired kidney function, such as those with chronic kidney disease (CKD), should use metformin with caution or under close medical supervision. In such cases, healthcare providers may adjust the dosage of metformin or consider alternative medications;
- Liver Function: Although metformin is not known to cause liver damage, it is essential to monitor liver function, especially in individuals with pre-existing liver disease or conditions that may affect liver function. Liver function tests may be conducted before starting metformin therapy and periodically thereafter to ensure the medication is well-tolerated;
- Lactic Acidosis: Lactic acidosis is a rare but potentially serious side effect associated with metformin use. This condition occurs when there is an accumulation of lactic acid in the bloodstream, leading to symptoms such as rapid breathing, muscle pain, weakness, and abdominal discomfort. Lactic acidosis is more likely to occur in individuals with conditions predisposing them to elevated lactate levels, such as kidney impairment or severe liver disease. It’s crucial to promptly seek medical attention if any symptoms of lactic acidosis develop;
- Vitamin B12 Deficiency: Long-term use of metformin has been associated with vitamin B12 deficiency, which can lead to anemia, neuropathy, and other complications. Regular monitoring of vitamin B12 levels and supplementation may be recommended for individuals taking metformin, particularly those with risk factors for deficiency, such as older age or a vegetarian diet;
- Drug Interactions: Metformin may interact with other medications, potentially affecting its efficacy or safety. It’s essential to inform healthcare providers about all medications, supplements, and herbal remedies being taken to avoid adverse interactions. Certain drugs, such as some antibiotics and contrast agents used in imaging procedures, may require temporary discontinuation of metformin to prevent kidney damage or lactic acidosis;
- Hypoglycemia: While metformin itself does not typically cause hypoglycemia (low blood sugar), combining it with other diabetes medications that lower blood sugar levels, such as insulin or sulfonylureas, may increase the risk of hypoglycemia. Close monitoring of blood sugar levels and adjustments to medication dosages may be necessary to prevent hypoglycemic episodes;
- Pregnancy and Breastfeeding: Metformin may be used to manage gestational diabetes under the guidance of a healthcare provider. However, the safety of metformin during pregnancy and breastfeeding is still being studied, and individual risks and benefits should be carefully considered in consultation with a healthcare provider.
Overall, metformin is a valuable medication for managing type 2 diabetes, but its use requires careful monitoring and consideration of individual health factors. By adhering to safety guidelines and working closely with healthcare providers, individuals can maximize the benefits of metformin therapy while minimizing potential risks.
Lifestyle Factors
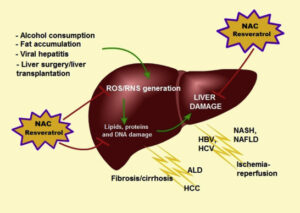
In addition to medication, lifestyle factors such as diet, exercise, and alcohol consumption can also influence liver health. Maintaining a healthy lifestyle, including a balanced diet and regular physical activity, can help support liver function and complement the effects of metformin therapy.
Conclusion
Metformin remains a stalwart ally in the management of type 2 diabetes, offering multifaceted benefits in blood sugar control and metabolic health. While concerns persist regarding its potential impact on liver function, current evidence suggests that metformin is generally safe and well-tolerated, particularly when used judiciously and with appropriate monitoring. By understanding the mechanisms of metformin’s action, staying vigilant about liver function, and adhering to safety guidelines, individuals can confidently navigate metformin therapy with the guidance of healthcare professionals.
As research continues to unfold, ongoing vigilance and collaboration between patients and providers will ensure the optimal balance between the benefits and risks of metformin, paving the way for improved outcomes and enhanced quality of life for individuals with type 2 diabetes.