Hep B Vaccination: Immunity Challenges Explained
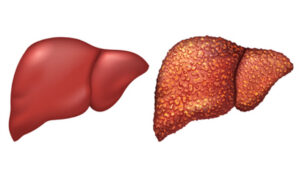
Hepatitis B, a liver infection that can lead to significant liver damage, is most commonly transmitted through contact with infected bodily fluids. While the hepatitis B vaccine significantly lowers the risk of contracting this infection, a small percentage of individuals, estimated between 5% and 10%, do not develop immunity after vaccination. These individuals are referred to as “non-responders.”
A non-responder to the hepatitis B vaccine is defined as a person who, after receiving at least two full doses of the vaccine, does not develop protective antibodies against the virus and has been confirmed through testing not to have either a chronic or acute hepatitis B infection. This article delves into the phenomenon of non-response to the hepatitis B vaccine, exploring its implications and the measures one can take to mitigate the risk of infection.
Hepatitis B can manifest as either an acute or chronic condition. Acute hepatitis B may resolve on its own without treatment, while chronic hepatitis B, although incurable, can be managed with medication to slow liver damage. In severe cases, chronic hepatitis B can lead to liver failure, necessitating a liver transplant. Symptoms of hepatitis B, which may not appear in all infected individuals, include stomach and joint pain, loss of appetite, nausea, fever, dark-colored urine, and yellowing of the eyes.
The Importance of Hepatitis B Antibodies
Antibodies play a crucial role in the body’s defense against hepatitis B. These blood proteins, produced by the immune system, help to identify and neutralize infections. Vaccines aim to stimulate the production of these reactive antibodies to provide immunity against the virus. However, non-responders, who do not develop these protective antibodies after vaccination, face an increased risk of hepatitis B infection.
Factors contributing to non-response include obesity, smoking, pre-existing chronic illnesses that weaken the immune system, and advanced age. For those who do not initially respond to the hepatitis B vaccination, further steps are recommended.
Steps for Non-Responders
- Testing: The first step involves testing for the hepatitis B virus to rule out an existing infection, which could explain the lack of response to the vaccine;
- Additional Vaccination: Non-responders who do not have hepatitis B may receive another round of vaccination, with a 30–50% chance of developing immunity after a second series of three doses. Subsequent testing will determine the success of this additional vaccination;
- Preventative Measures: Non-responders are counseled on reducing their risk of contracting and spreading hepatitis B. Recommendations include using condoms or other barrier methods during sex, regular testing for sexually transmitted infections, avoiding shared needles, practicing good hand hygiene, avoiding unprotected contact with bodily fluids, and seeking immediate medical care after potential exposure to the virus.
Non-responders can work in any role within healthcare settings, as the U.S. Occupational Safety and Health Administration (OSHA) mandates offering the hepatitis B vaccine to employees at risk of blood exposure and providing personal protective equipment. There are no regulations barring non-responders or those with chronic hepatitis B from employment in healthcare, although individual facilities may have their own policies regarding vaccination status.
To Wrap Up
In conclusion, while the hepatitis B vaccine is a crucial tool in preventing infection, non-responders must take additional precautions to protect themselves and others from hepatitis B. These measures, along with understanding the role of antibodies and the factors contributing to non-response, are essential in managing the risk associated with hepatitis B.
FAQs:
A hepatitis B vaccine non-responder is an individual who does not develop protective antibodies against the hepatitis B virus after receiving at least two full doses of the vaccine. This lack of immune response is confirmed through testing, which also ensures the person does not have an existing chronic or acute hepatitis B infection. Non-responders represent a small percentage of the vaccinated population but are at a higher risk of contracting hepatitis B due to the absence of immunity.
The reasons behind non-response to the hepatitis B vaccine vary and can include factors such as obesity, smoking, having a compromised immune system due to chronic illness, and older age. These factors may affect the immune system’s ability to produce antibodies in response to the vaccine, making some individuals more susceptible to non-response.
Non-responders should undergo testing to rule out existing hepatitis B infection. If negative, they may be offered an additional round of the vaccine. Regardless of vaccine response, non-responders are advised to practice preventative measures such as using barrier methods during sex, getting regular screenings for sexually transmitted infections, avoiding shared needles, maintaining good hand hygiene, avoiding unprotected contact with bodily fluids, and seeking immediate medical attention if exposed to the virus.
Yes, hepatitis B vaccine non-responders can work in healthcare settings. OSHA mandates that all employees exposed to blood be offered the hepatitis B vaccine and that personal protective equipment be provided. There are no regulations preventing non-responders or those with chronic hepatitis B from holding positions in healthcare. However, individual healthcare facilities may have their own policies regarding the employment of non-responders, which can vary but do not affect the individual’s ability to obtain a nursing license or secure employment in the field.