Cirrhosis-Linked Thrombocytopenia: Insights
Individuals with cirrhosis frequently experience thrombocytopenia, a condition characterized by a low platelet count. The reasons behind thrombocytopenia include factors such as spleen enlargement and diminished production of platelets. When thrombocytopenia becomes severe, it significantly elevates the likelihood of experiencing grave bleeding incidents.
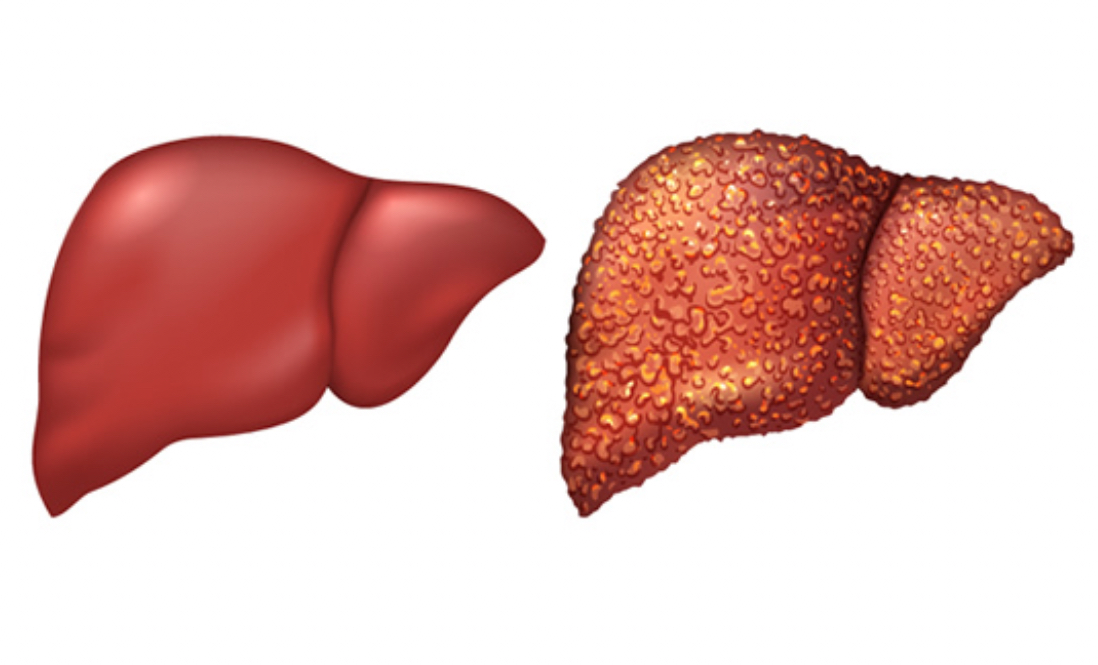
Cirrhosis is the result of permanent scarring of the liver, and statistics from the National Institute of Diabetes and Digestive and Kidney Diseases suggest that cirrhosis affects approximately one in every 400 adults in the United States. The compromised function of a cirrhotic liver leads to multiple health issues, among them thrombocytopenia, which manifests through symptoms such as easy bruising and bleeding.
This discussion will delve deeper into thrombocytopenia in the context of liver cirrhosis, covering its causes, diagnosis, treatment options, and the potential complications that may arise. Thrombocytopenia is a frequent complication in individuals suffering from chronic liver conditions, including cirrhosis, with around 70% of cirrhosis patients exhibiting varying degrees of this condition. The underlying causes of thrombocytopenia in cirrhosis are multifaceted and merit a closer examination.
Enlarged Spleen
The condition of cirrhosis significantly impacts the spleen, leading to its enlargement and subsequent trapping of platelets, which are crucial for blood clotting. This enlargement, a direct result of portal hypertension, highlights the interconnected nature of liver health and blood circulation. The process unfolds as follows:
- Cirrhosis Induces Portal Hypertension: Cirrhosis, through the formation of scar tissue, disrupts the normal flow of blood through the liver. This obstruction elevates the pressure in the portal vein, a key vessel supplying blood to the liver from various organs;
- Spleen Enlargement Occurs: The increased pressure in the portal vein leads to spleen enlargement. The spleen, acting as a blood filter, becomes overactive and starts to sequester more platelets than usual;
- Platelets Get Trapped: As the spleen enlarges, it traps platelets, preventing them from circulating in the bloodstream where they are needed for clotting. In severe cases, up to 90% of an individual’s platelets can be confined within the spleen.
This sequence of events underscores the critical role that liver health plays in maintaining proper blood circulation and clotting mechanisms. The trapping of platelets in the spleen not only highlights the severity of cirrhosis but also the body’s intricate response to such liver damage, resulting in significant clinical implications for individuals suffering from this condition.
Reduced Platelet Production
The liver’s compromised condition in cirrhosis can result in lower levels of thrombopoietin production, a crucial protein that signals the bone marrow to generate platelets, leading to a reduced platelet count. Other contributors to diminished platelet production include the impacts of chronic hepatitis B or C infection and excessive alcohol consumption.
Increased Platelet Destruction
Certain forms of cirrhosis may trigger an enhanced destruction of platelets due to the immune system erroneously targeting them. Autoimmune diseases or hepatitis C infections can initiate this immune-mediated platelet destruction. Diagnosis typically involves taking the patient’s medical history, conducting a physical examination, and ordering a complete blood count (CBC) to determine platelet levels. If cirrhosis is undiagnosed, additional tests may be conducted to confirm its presence and evaluate liver function.
Regarding treatment, several strategies exist to manage thrombocytopenia in cirrhosis patients, including medication to boost platelet production, platelet transfusions, spleen removal, splenic artery embolization, and the use of a Transjugular Intrahepatic Portosystemic Shunt (TIPS) to alleviate portal vein pressure. Preventative measures to mitigate cirrhosis progression include treating chronic hepatitis infections, abstaining from alcohol, maintaining a healthy weight in cases of nonalcoholic fatty liver disease (NAFLD), and using immunosuppressants for autoimmune liver diseases.
The primary complication of thrombocytopenia is the heightened risk of bleeding, either externally through skin injuries or internally following trauma. Portal hypertension can lead to varices in the esophagus or stomach, which are prone to bursting and causing significant bleeding. Severe thrombocytopenia complicates the management of cirrhosis and other health conditions due to the increased risk of bleeding during medical procedures.
Although thrombocytopenia is a common issue among cirrhosis patients, mild to moderate cases often do not require treatment. However, severe thrombocytopenia, defined as a platelet count below 50,000 per microliter of blood, poses a significant risk of serious bleeding. This condition not only complicates the management of cirrhosis but also indicates advanced disease and correlates with a poorer prognosis and increased risk of complications.
Table: Overview of Thrombocytopenia in Cirrhosis
| Factor | Description |
|---|---|
| Prevalence | Affects approximately 70% of individuals with cirrhosis. |
| Causes | Enlarged spleenReduced platelet productionIncreased platelet destruction |
| Symptoms | Easy bruising, bleeding |
| Diagnosis | Medical history, physical exam, complete blood count (CBC) |
| Treatment Options | Medication to increase platelet productionPlatelet transfusionsSpleen removalSplenic artery embolization Transjugular Intrahepatic Portosystemic Shunt (TIPS) |
| Prevention | Treat chronic hepatitisAbstain from alcoholMaintain healthy weight Use immunosuppressants for autoimmune liver diseases |
| Complications | Increased risk of bleeding, both externally and internally, especially in severe cases. |
This table encapsulates the critical aspects of thrombocytopenia in the context of liver cirrhosis, offering a structured overview of its impact, management, and the imperative for preventative care.
Conclusion
In conclusion, thrombocytopenia presents a significant challenge in the management of liver cirrhosis, impacting a large proportion of patients with this liver condition. Its multifactorial etiology, encompassing spleen enlargement, reduced platelet production, and increased platelet destruction, underscores the complexity of cirrhosis as a disease and its systemic effects. Effective management of thrombocytopenia requires a comprehensive approach, including both preventive strategies to slow the progression of cirrhosis and specific treatments aimed at mitigating the low platelet count. Advanced diagnostic tools and a range of treatment options, from medication to surgical interventions, play a crucial role in improving patient outcomes. While the irreversible damage of cirrhosis poses an ongoing challenge, understanding and addressing thrombocytopenia can significantly reduce the risk of severe complications, thereby enhancing the quality of life for those affected.
FAQs:
Thrombocytopenia is a medical condition characterized by an abnormally low number of platelets in the blood, crucial for the clotting process. In the context of cirrhosis, thrombocytopenia often arises as a complication due to the liver’s diminished ability to produce thrombopoietin, a key growth factor for platelet production. Furthermore, cirrhosis can lead to portal hypertension, causing the spleen to enlarge and sequester a significant portion of the body’s platelets, thereby reducing their availability in the bloodstream. This relationship between cirrhosis and thrombocytopenia highlights the liver’s integral role in blood regulation and the complex interplay between liver health, spleen function, and blood cell production.
Thrombocytopenia in patients with cirrhosis is primarily diagnosed through a complete blood count (CBC) test, which measures the levels of various blood cells, including platelets. A CBC test is conducted using a blood sample taken from a vein, typically in the arm. If the platelet count is found to be lower than the normal range, it suggests thrombocytopenia. For patients not previously diagnosed with cirrhosis but suspected of having the condition due to low platelet counts, doctors may recommend additional tests. These can include liver function tests, blood clotting tests, imaging tests (such as ultrasound or MRI), and possibly a liver biopsy to assess the extent of liver damage and confirm the presence of cirrhosis.
counts and addressing the underlying liver condition. Treatment options include:
1. Medications: Drugs like avatrombopag, eltrombopag, lusutrombopag, and romiplostim can stimulate the bone marrow to produce more platelets.
2. Platelet Transfusions: This involves transfusing platelets from a healthy donor to the patient to temporarily increase platelet counts, particularly in cases of severe bleeding or before a surgery.
3. Spleen Removal (Splenectomy): In some cases, removing the spleen can prevent platelets from being sequestered, thereby increasing their number in the bloodstream.
4. Splenic Artery Embolization: This procedure reduces blood flow to the spleen, diminishing its size and the amount of platelets trapped.
5. Transjugular Intrahepatic Portosystemic Shunt (TIPS): TIPS can alleviate portal hypertension, indirectly reducing spleen size and improving platelet counts.
Treatment choice depends on the severity of thrombocytopenia, the underlying cause, and the overall health status of the patient.